The world of health is never at a loss for important, cutting-edge topics. So, we let four highly respected Valley doctors hold the writing reins, asking them to explain what they believe is a leading health care topic of the times. From e-medicine to stem cell transplants, here’s what they had to say.

Breast Brachytherapy Leading Cancer Treatment Revolution
Did you know that more than 4,000 women in Arizona will be diagnosed with breast cancer this year? With such a large population of both survivors and newly diagnosed breast cancer patients, quietly over the past several years, some of the most exciting research and clinical trials surrounding breast cancer treatment and technology have been taking place right here in Arizona—in our own backyard.
Among the most exciting has dealt with breast brachytherapy, which is a five-day radiation therapy alternative for women with early stage breast cancer. The procedure places radiation sources—usually tiny pellets the size of pencil lead—inside and adjacent to a cancer or inside an area that may contain residual cancer after surgical removal of the visible tumor mass. Using brachytherapy, doctors can reduce the radiation exposure to nearby normal tissues that do not need—and can be harmed by—the radiation.
The beauty of breast brachytherapy lies in the laws of physics. While very close to the radioactive seeds, the radiation intensity is very high; however, just millimeters away, the seeds’ radiation intensity decreases dramatically. This law of physics gives us a therapeutic advantage; if the seeds are precisely positioned in the tissues containing cancer cells, the normal tissues including the lungs, heart, ribs and skin can be avoided.
Another bonus—especially in a Silicon Valley like Scottsdale—breast brachytherapy can be used to treat women with breast implants as well. All too often, doctors recommend mastectomy for augmented women who have been diagnosed with breast cancer, primarily because long courses of traditional radiation can harden implants. Since very little of the implant receives radiation exposure via brachytherapy, the scar tissue does not wrap around the silicone or saline implant, thus avoiding the shrinkage and hardening altogether—not to mention the long recovery process involved with a mastectomy.
Given the level of success of this treatment option, today I am proud to serve as co-principal investigator in the largest breast cancer radiation trial in medical history, squarely focused on breast brachytherapy. This trial, sponsored by the National Cancer Institute, has now completed testing 4,300 women. Six-week whole breast radiation is compared head-to-head with our five-day breast brachytherapy.
We believe the results, once analyzed and presented in coming months, could inspire the biggest paradigm shift in how patients will be treated since Marie Curie herself discovered radium in 1896.
Dr. Robert Kuske is the original pioneer of breast brachytherapy treatment, a technique he invented in 1991. He is a partner at Arizona Breast Cancer Specialists and is providing radiation oncology services at its facility on Scottsdale Healthcare’s Virginia G. Piper Cancer Center campus.

Improving Health Electronically: Benefits of Electronic Health Records
How can electronic health records improve a patient’s health? When a network of providers have access to medical records that can be easily shared, that’s how. Just imagine the efficiency, time savings, cost savings and even the possible life-saving information that is at the doctor’s fingertips in event of an emergency.
John C. Lincoln Health Network launched its electronic medical record, JCL Connect, in March 2012. With the vast number of primary care locations, hospitals, medical imaging offices, labs and other facilities in the Valley, establishing one record for each patient that can be easily shared speaks volumes. Having one record allows John C. Lincoln doctors to offer efficient care to their patients; they can see labs, procedures and consult notes from specialists and provide optimal care based on all the information they have access to in their electronic record.
Not only do our electronic medical records allow our physicians to provide more efficient care, but patients of the John C. Lincoln Physician Network can access their personal health care records via the patient portal, JCL MyChart.
With JCL MyChart, patients can manage their health information from a computer, tablet, iPhone or Android at any time. Advantages include receiving many tests and lab results online with no waiting for a phone call or letter; reviewing your medications, allergies, immunizations and health history; requesting and confirming appointments; requesting prescription refills; conveniently and securely messaging staff at your health care provider’s office, from the health care provider to the medical assistant to the billing office; and reviewing health education topics and post-visit instructions provided by your health care provider.
You also can link your children’s or elderly parents’ accounts to your own for convenient access to their appointments, immunization records, growth charts and more.
Aaron Boor D.O. is the lead physician builder of JCL Connect. jclmychart.com
Before Playing Ball: Baseline Concussion Testing
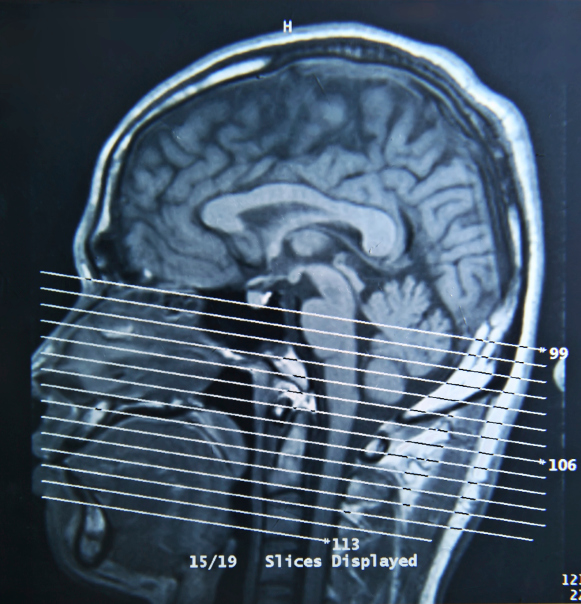
As knowledge about the dangers of concussions in sports continues to grow, Mayo Clinic has made baseline concussion testing available at no cost to all middle and high school students in Arizona.
Baseline concussion testing measures how the brain is working before injury. The testing tool is available through the generous support of the J. Theodore Curtis Karalis Foundation and Mayo Clinic at no cost. The test can be taken from any computer with Internet access, takes eight to 15 minutes, and the athlete or parent can share the results with health care providers of their choice. (Test can be accessed at www.mayoclinic.org/concussion-testing.) After a concussion, the test can be repeated as often as necessary, and along with a medical evaluation by a concussion expert, the results can be used to help guide return-to-play decisions.
This initiative comes on the heels of Arizona Senate Bill 1521, which requires that high school athletes who have sustained a head injury be barred from further physical activity until they're cleared by a licensed health care provider. The law also requires schools to educate coaches, students and parents about the dangers of concussions.
So why is this important? The diagnosis of concussion, assessment of severity, and knowing when an athlete can return to play, work or school is not always clear. This kind of assessment for each athlete will provide the health care provider with often the only objective tool that indicates when an athlete’s brain has truly returned to his or her baseline. Baseline concussion testing has been mandatory for many years for all Olympic, NCAA Collegiate, and many professional (NHL, NFL, MLB) athletes. Concussion experts at Mayo Clinic believe that if such a test should also be mandatory for youth athletes as well.
After a concussion, if an athlete continues to play or returns to play too early, there’s a significant risk of experiencing another concussion, and repeat concussions may take longer to resolve, and come with a risk of permanent neurological damage, or rarely, death. Children, adolescents and female athletes appear to be at a higher risk and may take longer to recover.
While the importance of baseline testing is clear, the results should be used with a comprehensive medical evaluation. The medical care and rehabilitation of athletes whose symptoms are persistent is best achieved by a multidisciplinary team of health professionals with expertise in the evaluation and management of concussion.
David Dodick M.D. is a neurologist with Mayo Clinic. An internationally recognized migraine expert, Dr. Dodick is the past president of the American Headache Society, president-elect of the International Headache Society, vice-chair of the World Federation of Neurology Headache Research Group, editor in chief of Cephalalgiaand director and founder of the Headache and Concussion Programs at Mayo Clinic in Arizona.

Saving With Stems
More and more, the use of stems cells in medical research and treatment is making a huge difference in patient care. Today, at the Stem Cell Transplant and Cellular Therapy Program at Banner MD Anderson Cancer Center, we are applying this treatment and making a difference in the patients we treat.
Patients often ask: “Are stem cell transplants right for me?” It’s a great question. To determine if a stem cell transplant is an effective treatment option for cancer, it’s important to understand how the process works. Bone marrow is made of stem cells which produce red cells to carry oxygen to tissues, white cells to fight infections, and platelets to prevent excessive bleeding. If bone marrow is damaged or invaded by cancer, the number of healthy stem cells is significantly reduced, which can cause fatigue, bleeding and problems fighting infection. A stem cell transplant can repopulate the bone marrow and allow new stem cells to develop.
In cancers of the bone marrow or lymph nodes, high doses of chemotherapy or radiation can be the most effective treatment to kill cancer cells. However, this same treatment can also destroy healthy bone marrow, so a stem cell transplant replenishes the cells lost from the chemotherapy or radiation. This is called autologous stem cell transplantation and involves collecting the patient’s own stem cells before treatment to use as rescue after a high dose of chemotherapy.
A stem cell transplant may also be used to treat cancer directly. Stem cells from another person, typically a matched sibling, have a powerful effect in killing cancer cells. In this situation, the donated cells are transplanted to actually fight the cancer in addition to replacing the old bone marrow. This type of stem cell transplantation, called allogeneic, is used for treating most forms of leukemia.
Though a stem cell transplant has great healing potential, it is not risk-free. Therefore, a patient’s care team must evaluate the benefits and risks of the transplant relative to the patient’s age, organ functions, type of cancer and status of the disease to determine if this treatment is optimal.
Gorgun Akpek M.D. is the director of the Stem Cell Transplant and Cellular Therapy Program at Banner MD Anderson Cancer Center.
Story by Melissa Larsen